In the last article, we charted how potentially pathogenic mutations could be carefully sifted out from a large pool of somatic variations. The final, most important part is figuring out how this information can be used to make the best treatment decisions for the patient.
Cancers arise, progress, and spread due to the uncontrolled, chaotic multiplication of cells, accumulating more and more mutations in the process. The more advanced the cancer, the higher the number of genetic variations it can accrue. Sequencing the tumor reveals the entire constellation of mutations carried within it, and the classification process identifies those with the potential to cause harm—either by promoting unchecked cell division or by making the cancer resistant to certain types of treatment. These may include variants linked with approved drug targets and those still under research. Every day, new discoveries in cancer therapy are made. Since 2018, more than 120,000 clinical trials have been registered on ClinicalTrials.gov, and the FDA has approved over 200 drugs. Every year, thousands of research papers on cancer biomarkers are published [1].
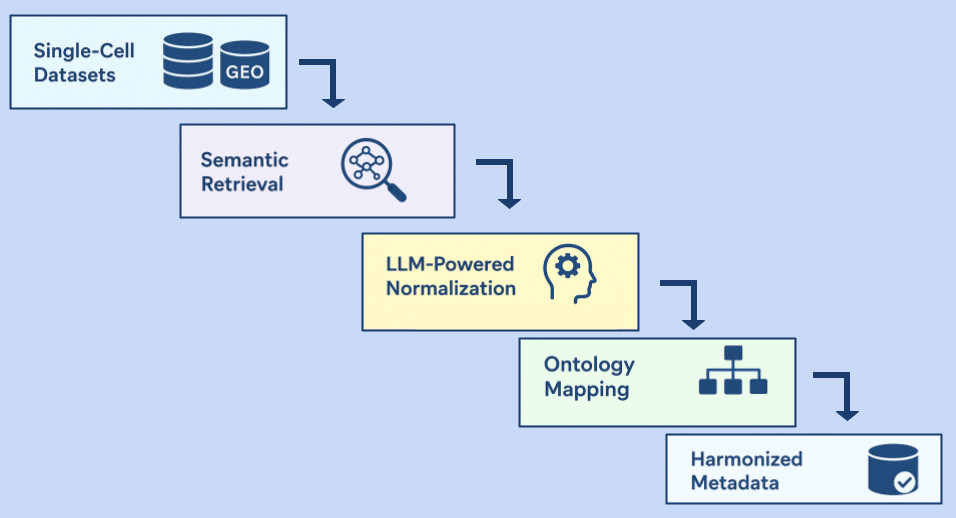
Therefore, what would really be useful is a robust algorithm that can connect each variant to all potential treatment options, allowing clinicians to get an overall picture of the routes they can consider. Most databases have search tools that can retrieve some of this information, but it is not always best utilized. Therapy suggestions in somatic variant reporting rely on independent variant-drug associations to assess drug response. Although this method is somewhat helpful, it can also lead to a misunderstanding of the patient's drug sensitivity. This is because a patient might seem to respond well to a drug due to a certain variant, but other variants that either resist or enhance sensitivity could change the effectiveness of this response.
For example, in the case of a patient with non-small cell lung cancer (NSCLC) who has the EGFR (epidermal growth factor) L858R variant, the response to the drug erlotinib might appear positive. However, if the patient also has the EGFR T790M variant, known for resisting erlotinib treatment, the overall positive response is significantly reduced. Reporting these associations separately won’t provide an accurate picture of their erlotinib response.
StrandIris is a platform that can address these needs in a uniquely effective way, as it provides a comprehensive profile of the patient’s drug response. Its intricate rule-sets factor in the entire combination of variants in the patient, considering multiple variant-drug connections and finally producing a single recommendation showing the overall likelihood of drug response. For the example above, both EGFR L858R and EGFR T790M are considered to assign a final 'poor' overall response to erlotinib.
While other databases mostly have information on approved drugs, with a few investigational drugs or clinical trials, StrandIris taps into an exhaustive database of investigational drugs and clinical trials. It organizes drugs into drug classes, including both widely studied drugs and lesser-known but promising ones, giving patients a broad range of treatment choices and options. Clinical trials from both US clinicaltrials.gov and WHO ICTRP are incorporated into the Strand Iris tool, to cover trials being conducted around the world. Variants are matched with clinical trials nearest to the patient’s geographical location, and annotated with AMP tier as per evidence. This information is updated regularly, and drug approvals are immediately added.
For instance, the Poly ADP ribose polymerase (PARP) inhibitor olaparib is widely considered for Ataxia-telangiectasia-mutated (ATM) cancers. Niraparib, a drug of the same class, is not as widely studied. In its report, Strand Iris considers recommending niraparib along with olaparib, with relevant information about evidence from clinical trials.
Once generated, the patient is matched with a genetic counselor to unpack the report and understand the various ways forward. The entire path from detection to prognosis can be optimized for the patient on the same platform, which makes Strand Iris a new frontier in precision oncology.
You can find more details regarding StrandIris, here!
Explore the rest of the blog series below:
- Part 1: Precision Oncology: A Genetics Revolution in Cancer Management
- Part 2: Somatic Variants and Databases: A Wealth of Information
- Part 3: Somatic Variant Classification—Mining for Clues
References:
- O. of the Commissioner, “U.S. Food and Drug Administration,” FDA, Aug. 21, 2023. https://www.fda.gov/ (accessed Aug. 22, 2023).