Australian actor Chris Hemsworth was recently informed by his doctor that he was 8–10 times more likely to develop Alzheimer’s disease, a neurodegenerative disease characterized by the loss of memory and other important mental functions. This risk was ascertained based on Hemworth’s genome sequence, in particular from two copies of a genomic variant in his APOE gene, a well known risk gene. This adds to the list of high profile cases where genomic variants have predicted a much higher than baseline long term risk even when the individuals in consideration have no sign of disease currently. Sergei Brin, the Google co-founder, stands a >50% risk of developing Parkinson’s disease, the degenerative central nervous system disorder, because of a genomic variant in the LRRK2 gene. Angelina Jolie, the popular actress, had an 87% chance of breast cancer and >50% of ovarian cancer on account of a genomic variant in the BRCA1 gene, until she had elective surgeries to reduce her risk.
Alzheimer’s disease (AD) occurs most often in people above 65, and 80% of affected individuals are 75 or older. The disease is progressive, with increasing loss of normal brain function with time. 50m people suffer from AD worldwide. The estimate for India is ~3m, perhaps lower than expected on account of our young demographic, but certainly likely to grow as life expectancy grows. The Global Burden of Disease study published in the Lancet Public Health predicts a tripling by 2050.
The causes of AD are being actively researched. Studies on post-mortem brains from AD patients have shown a toxic plaque build up between the neurons caused by clumping of a molecule called beta-amyloid. Inside the neurons, there are abnormal tangles caused by clumping of a protein called tau. Finally, there are cells called microglia that engulf and destroy waste and toxins in the normal brain, but are somehow compromised in the AD brain. The question then becomes: what causes this plaque build-up between neurons, the tau tangles within neurons, and the compromised microglia, in AD brains? How much of this cause lies in our genes and how much is a function of our lifestyle and environment, which we can perhaps influence more than our genes?
Studies on twins who have the same genomes but different environmental influences suggest that at least 50% of the “causative burden” lies in the genes. The first few genes to be causative of AD were discovered in the 1990s by studying families who had a very early onset of AD (in the 40s and 50s, instead of late 60s). These include the Amyloid protein precursor (APP), presenilin-1 (PSEN1), and presenilin-2 (PSEN2) genes. Typically, we have two copies of most genes, with one copy protecting us in the event where the other is rendered ineffective by a genomic variant. However, certain rare variants in even one copy of these genes turn out to be causative of AD. Even then, such variants are rare and certainly not present in most patients with AD. Where in the genome does the cause lie for these AD patients?
Chances are the genomic cause lies in what are called common variants. As the name indicates, these are genomic variants that are present in many people, not all of whom will go on to develop AD. Unlike rare variants in the previous paragraph, which act single-handedly and are overwhelming in their effect, each common variant is subtler and acts in concert with many other common/rare variants and with other environmental causes. To tease apart the effect of such common variants is therefore not easy. However, over the last decade or so, so-called Genome Wide Association studies run on >100,000 AD patients have yielded some common variants that seem to occur more often in AD patients than in others. Of these, the strongest such common variant is the so-called ApoE-ε4 variant in the APOE gene. This is precisely the variant found in Hemworth’s genome.
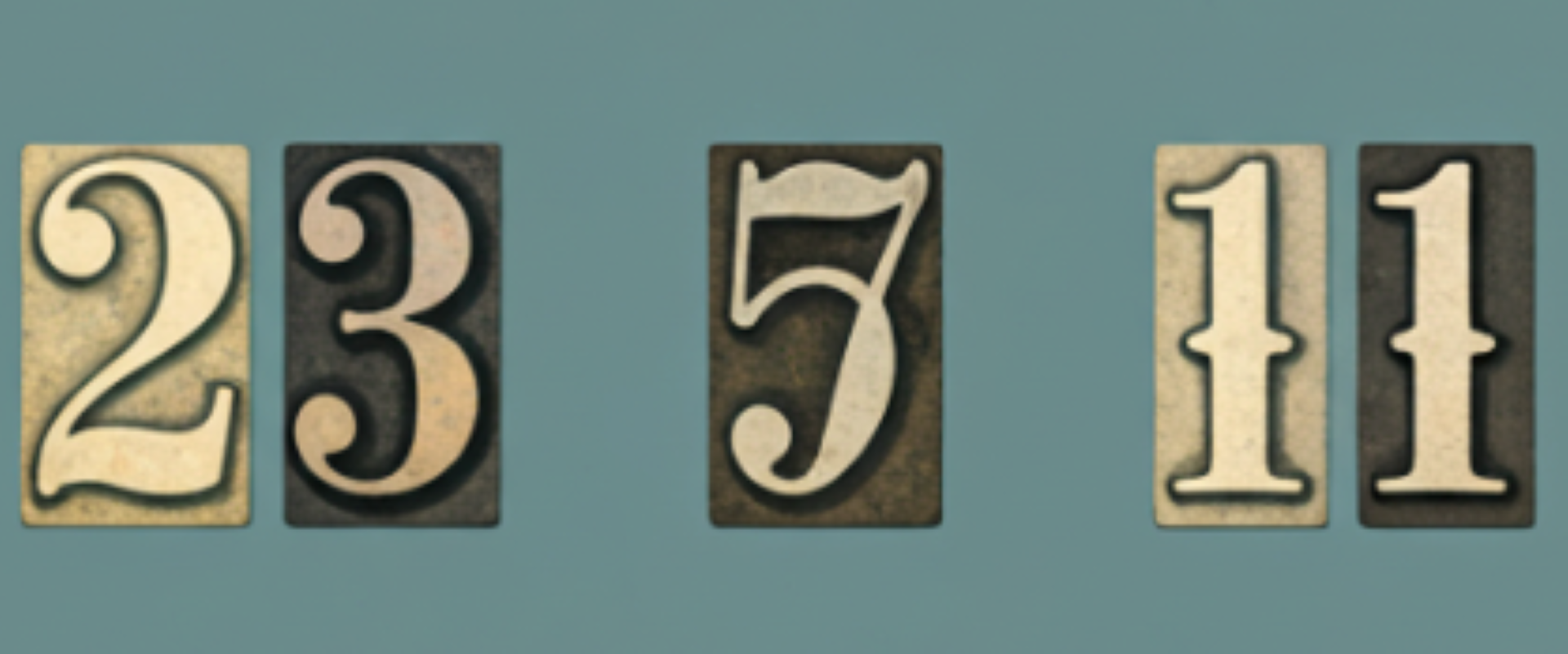
~25% of all humans and 60% of all AD patients carry at least one copy of ApoE-ε4. Not all these individuals will go on to develop AD, because only some will have the right combination of the several common variants and environmental factors involved. A comprehensive analysis of the combined effects of all these variants and factors is not yet possible, so, we can talk today only about risk and increased odds. Each copy of ApoE-ε4 is associated with a roughly threefold increase in the odds of developing AD. Hemsworth has two copies, which make his odds 8–10 fold that of a normal person.
Note again that Hemsworth’s odds are 8–10 fold that of a normal person on account of ApoE-ε4. He may have other common variants in his genome that could modulate this risk upwards or downwards. For instance, two common variants in the KL gene can dial down the risk a bit, while another not uncommon variant in the TREM2 gene can dial the risk further upward. At the current state of the art, while we can identify most of Hemsworth’s genomic variants, we cannot yet predict how the combination of all these variants might modulate his 8–10 fold risk. Of course, the fact that his grandfather also had AD suggests that he may have inherited some more common variants that add to his risk.
How can Hemsworth tweak his environmental or lifestyle factors to manage his risk when he enters his 50s and 60s? While there aren’t clinically proven ways, research on this question is advancing. First, there are proteins in his blood that he could measure (P-tau181, P-tau231, Aβ42/40, NfL) that provide advance warning on degeneration in his brain 10 years prior to any symptoms becoming visible. Second, recent studies have shown some evidence that supplementation with docosahexaenoic acid, an omega-3 fatty acid naturally found in fish, could delay the onset of AD, particularly in those with the ApoE-ε4 genomic variant, which includes Hemsworth. Of course, a generally healthy lifestyle balancing dietary components and exercise is only expected to help.
The discovery of drugs to slow down or cure AD has turned out to be a tough exercise. While there has been little success so far (only one conditional US FDA approval), there are 143 agents under clinical development in 172 clinical trials, as of Jan 22 (phase 1: 30 agents, phase 2: 82 agents, phase 3: 31 agents). Several lessons have been learnt from failed clinical trials and it is now clear that an antibody-based drug, when given in high enough doses, can bring the levels of toxic beta-amyloid plaque in the brain down to very low levels. Hopefully, there is now light at the end of this tunnel. And, Hemsworth has time on his side for this to play out.
In addition, the number of individuals whose genomes are sequenced is expected to accelerate at an unprecedented rate in the near future thanks to costs that continue to decline. As that happens, it may become possible to determine Hemsworth’s risk more finely as well.

27 Mar 2023
Chris Hemsworth and the risk of Alzheimer’s Disease
WRITTEN BY
Dr. Ramesh Hariharan
Today’s Pick
from Blogs
from Blogs
13 Sep 2024
FDA Rule on Lab Developed Tests (LDTs)3 | Partnering with New Molecular LDTs: Strand's FDA Compliance Roadmap
Divya Anantsri
Know More